Why your hip labral tear diagnosis shouldn’t scare you.
Jun 07, 2022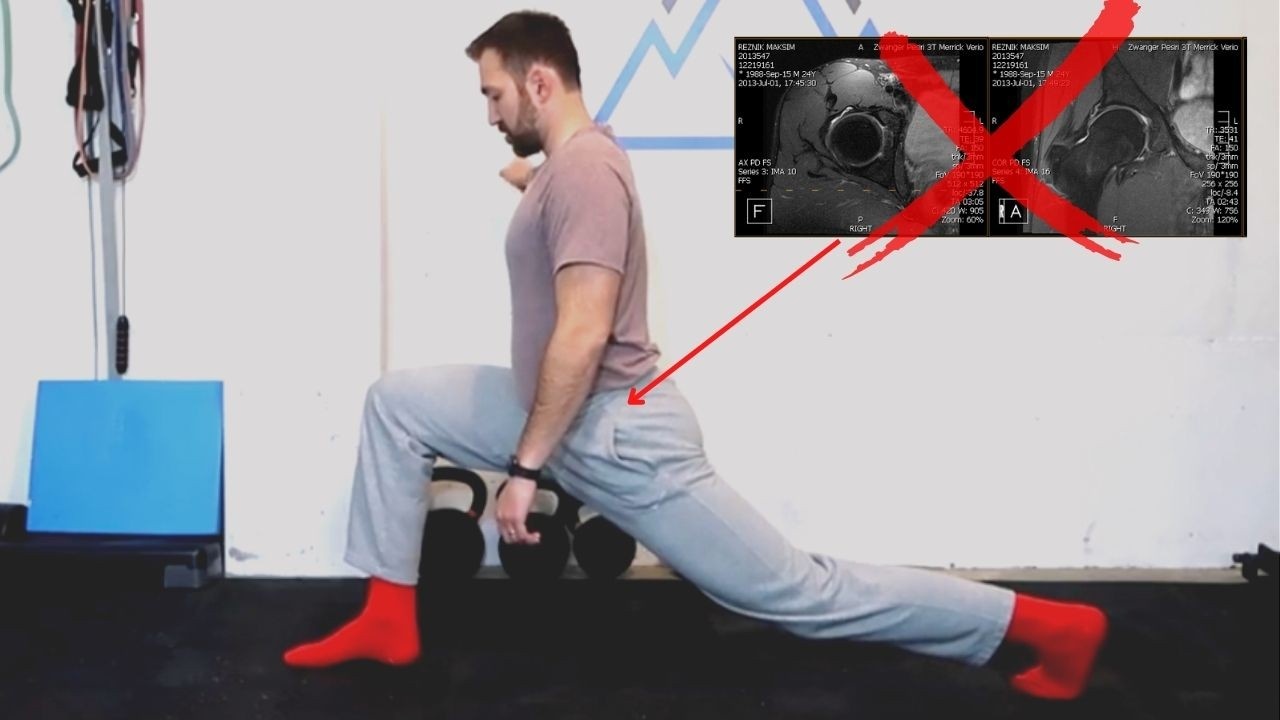
Have you been diagnosed with a hip labral tear but don’t know what to do about it? Should you get steroid injections or physical therapy? Do those things even work? And if they don’t work, does that mean you need surgery?
Surgery!? Did your hips get so screwed up from wear and tear that you now need to go under the knife? No they did not. In this article, I’ll explain why you shouldn’t fear a hip labral tear diagnosis and why it’s not what's behind your chronic hip pain.
How would I know? Because I was where you were. I was diagnosed with a hip labral tear over a decade ago. I went through all the conventional treatments - physical therapy, injections - and even experimented with the alternative treatments - chiropractor, diet change, yoga and a bunch of other things.
And I was 2 days away from getting surgery before I decided to cancel the procedure. Instead of getting surgery, I began exploring the world of movement. I relearned how to move my hips. I rebuilt my hip function. And I integrated this with how my body moves globally.
10 years later, I have no hip pain and I’ve helped hundreds of people diagnosed with hip labral tears get out of chronic hip pain. If you’re reading this, you might have some doubts about your hip labral tear diagnosis. Your doubts are rational. And I hope the below information validates your concerns and gives you some direction in your journey out of chronic hip pain.
What is a labral tear of the hip and does it cause pain?
Let’s start from the beginning shall we? Let’s examine how the medical community defines a hip labral tear.
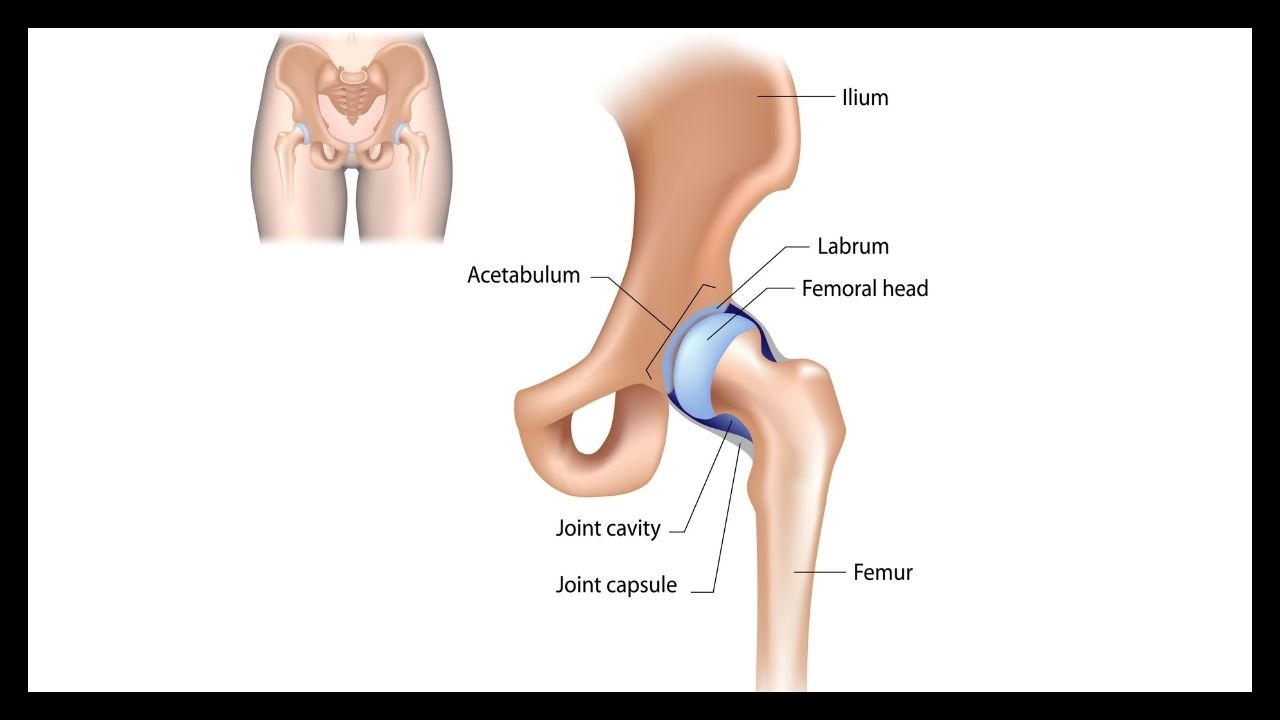
- From the Cleveland Clinic: “The hip is shaped like a ball-and-socket. The socket is called the acetabulum, and the ball is the femoral head, located at the top of the femur (leg bone). A hip labral tear is an injury to the labrum, the soft tissue that covers the acetabulum.”
- From the Mayo Clinic: “A hip labral tear involves the ring of cartilage (labrum) that follows the outside rim of the hip joint socket. Besides cushioning the hip joint, the labrum acts like a rubber seal or gasket to help hold the ball at the top of the thighbone securely within the hip socket. Athletes who participate in sports such as ice hockey, soccer, football, golf and ballet are at higher risk of developing hip labral tears. Structural problems of the hip also can lead to a hip labral tear.”
The Mayo and Cleveland clinics are highly reputable medical organizations. And rightfully so. They provide trusted information to the public about medicine and health. And I have nothing bad to say about them.
BUT as with many things in life, nuance exists in this diagnosis. And it is not the responsibility of the Mayo Clinic or Cleveland Clinic or any other institution that dominates Google SEO to provide all of the nuance that exists in a particular medical condition.
As we go through various sub-topics on hip labral tears, I will share with you the nuances that exist in this condition. I’ll explain where there is important information that is not usually provided by major medical institutions. Because it’s important for you to have all of the necessary information before deciding how to treat your hip(s).
The first and most important piece of information is that many people with hip labral tears are asymptomatic. In other words, many people have hip labral tears but no hip pain. Here are some studies to bring home this point:
- 89% of young athletes with no history of hip pain had hip labral tears. [Link to study].
- 69% of study participants with no history of hip pain had hip labral tears. [Link to study].
- 57% of asymptomatic volunteers had hip labral tears. [Link to study].
- 45% of young healthy asymptomatic volunteers showed evidence of labral pathology. [Link to study].
Why do these studies matter? Because it demonstrates that hip labral tears are very common in the general population. A tear in the labrum does not mean pain in the hip. This is so important and I cannot stress it enough.
This is the type of nuance that is critical to know when learning about your hip labral tear diagnosis. If you leave with nothing else from this article, let this get implanted into your brain: you can have a hip labral tear and not be in hip pain; you can also have hip pain and not have a hip labral tear.
A hip labral tear feels different for everyone
Every “body” is different and variation is expected with any health issue. But, usually there is some type of consistent pattern of symptoms that help identify a particular condition. For example, not only did I once have chronic hip pain, I was also blessed with gout.
The symptoms of gout are unmistakable. You wake up in the middle of the night with excruciating pain in the bunion joint of the big toe. You thought your hip pain was bad? Man, there is nothing quite like the pain experienced during a gout flare up.
And of course there is some variation in the types of symptoms people get during a gout flare up. How red the toe gets. The severity of the pain. How long the flare up lasts. What helps with the local inflammation. Etc. But if you show a rheumatologist or podiatrist your foot, they’ll tell you it’s gout within seconds.
The same cannot be said about hip labral tears. The symptoms vary greatly by individual and there is a lack of consistency in the medical literature. Let’s examine this further.
There is a Wide Variety of Hip Labral Tear Symptoms
As many of us know, using google to self-diagnose is a slippery slope. This slope gets even more slippery when the list of symptoms lack any uniformity. Here is a short list from Google when searching for “hip labral tear symptoms:”
- Pain in the hip or groin often made worse by long periods of standing, sitting or walking or athletic activity. [Mayo Clinic].
- A locking, clicking or catching sensation in the hip joint. [Mayo Clinic].
- Stiffness or limited range of motion in the hip joint. [Mayo Clinic].
- Pain in the . . .buttocks, especially as you walk or run, and sometimes at night when you sleep. [Hopkins Medicine].
- Sharp pain in the front of the hip. [University of Utah].
- Feeling unsteady on your feet. [Cleveland Clinic].
So let’s summarize this. Symptoms for a hip labral tear can be in the hip joint, groin, front of the hip and buttocks. It can come on during standing, sitting, sleeping, walking, running, or other forms of athletic activity. Sensations experienced include locking, clicking, catching, sharpness and feeling unsteady on your feet.

Hip labral tear pain can allegedly be anywhere in or around the hip. And the type of sensation experienced can also vary greatly. Unlike a condition like gout where symptoms are overwhelmingly obvious, the same cannot be said about hip labral tears.
Hip Labral Tear Pain Patterns Have no Consistency
Not only do symptoms vary but so do the pain patterns for hip labral tears. In my own case, when I first started getting pain, I thought it was more of a low back problem than a hip problem. I felt a dull ache that radiated from my low back all the way to my lateral hip.
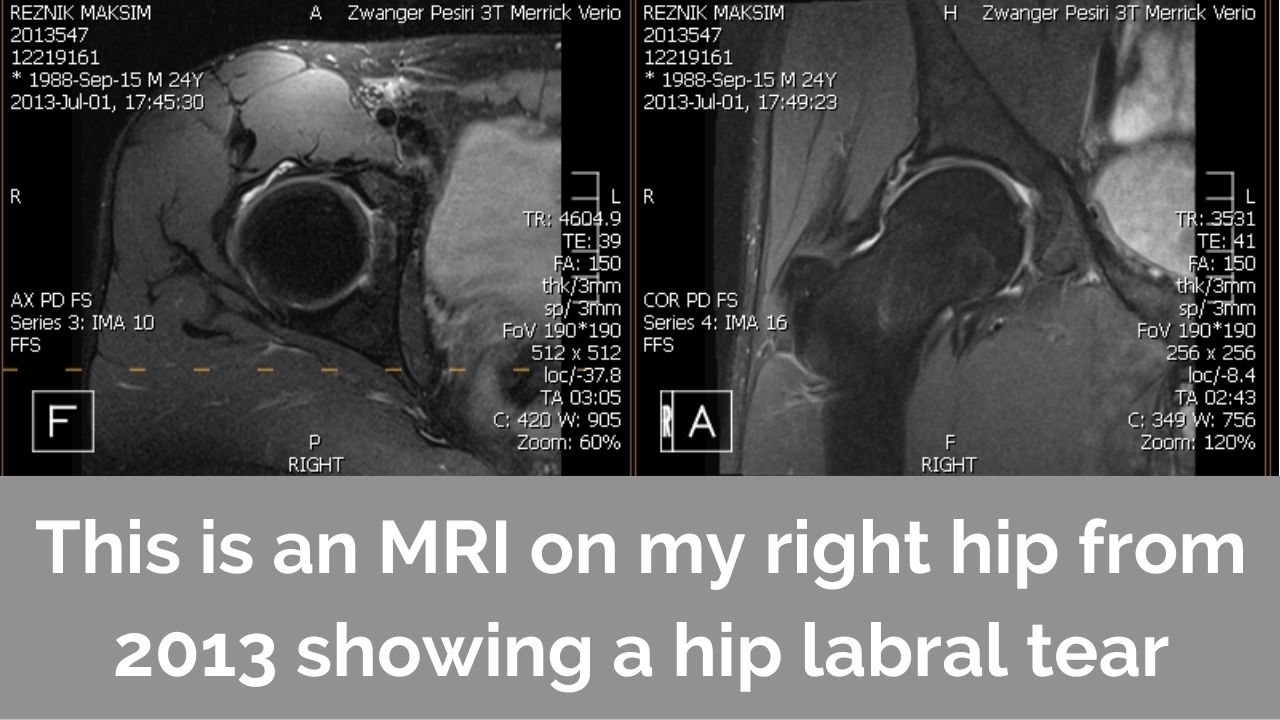
After some medical professionals convinced me it was my hip and not my back, I ended up getting an MRI on my hip. And this led me to receiving a hip labral tear diagnosis. But when I read about other people’s experiences, I didn’t relate to what they were feeling.
People were describing their discomfort as pinching in the front of the hip or groin. I only started doing my initial research but already the doubts were forming. Over a decade later, I see the exact same thing with clients I work with that were diagnosed with hip labral tears.
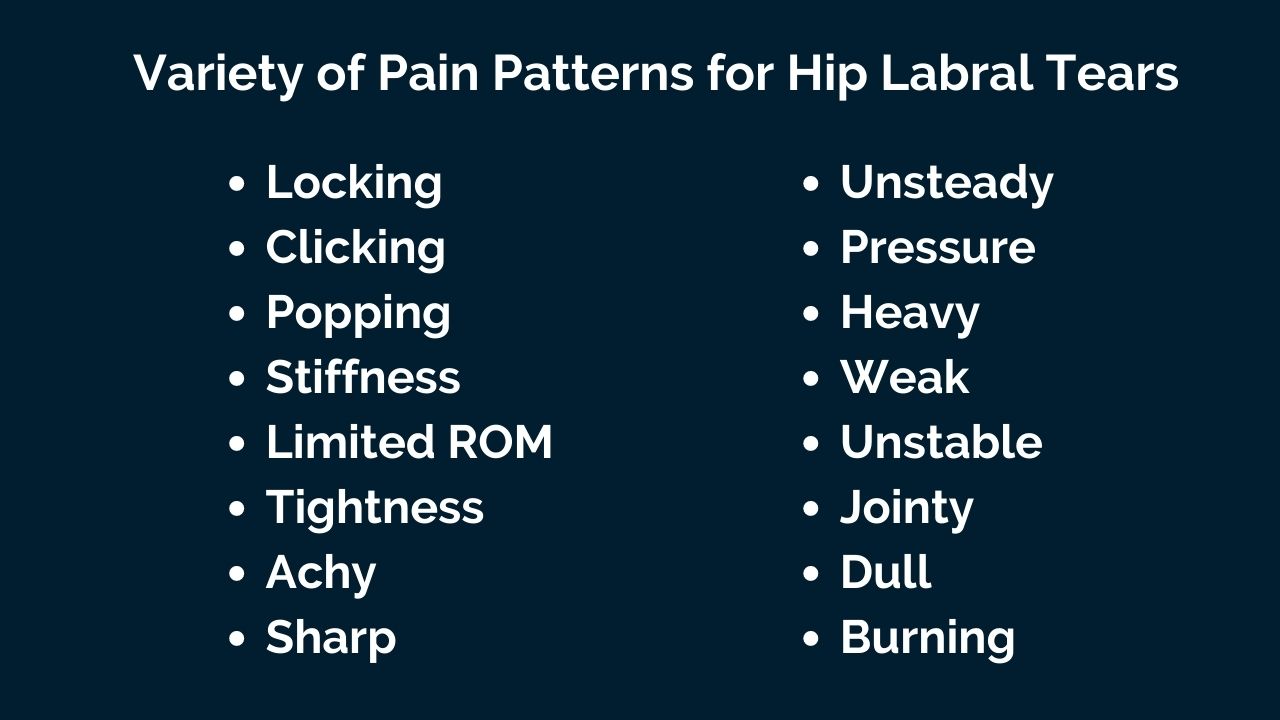
There is zero consistency in the pain patterns. Some people have sharp pain while others have dull pain. Some have a consistent ache while others have periodic episodes of discomfort. Some feel the pain in the groin while others feel it in the side of the hip.
Taken in isolation these anecdotal examples from my clinical experience might not be convincing. But it’s not the only issue in the hip labral tear diagnosis. As we’ve learned, there is no connection between hip pain and a hip labral tear.
Now we are learning that there is no uniformity in symptoms or pain patterns in those diagnosed with hip labral tears. And as we’ll see, the issues continue once we start examining the testing and treatment for hip labral tears.
Why Tests for Hip Labral Tears do not Work
We now know that hip labral tears may not cause pain and that there is no uniformity in symptoms or pain patterns with those diagnosed with this condition. But there must be some reliable way to test for hip labral tears right? If there is a trustworthy and repeatable way to confirm a hip labral tear is causing pain then all the other stuff doesn’t matter right?
Well comrade, unfortunately there is not. Each main testing method is incredibly flawed. Below, we will look at each of these testing methods in detail. As you’ll see, none of these tests have the reliability one would expect before getting diagnosed with a serious medical condition.
Why Hip Labral Tears on MRI Scans do not Tell the Whole Story
As I explained in the first section of this article, many people have hip labral tears but no pain. I will plug in the studies from before here as well. In each of these studies, all of the volunteers had NO hip pain but had a hip labral tear diagnosis. Here they are again:
- 89% of young athletes with no history of hip pain had hip labral tears. [Link to study].
- 69% of study participants with no history of hip pain had hip labral tears. [Link to study].
- 57% of asymptomatic volunteers had hip labral tears. [Link to study].
- 45% of young healthy asymptomatic volunteers showed evidence of labral pathology. [Link to study].
In the study of young athletes, 89% of asymptomatic hips had hip labral tears! Are we going to operate on a 16 year old hip because of a hip labral tear when there is no pain? Of course not.
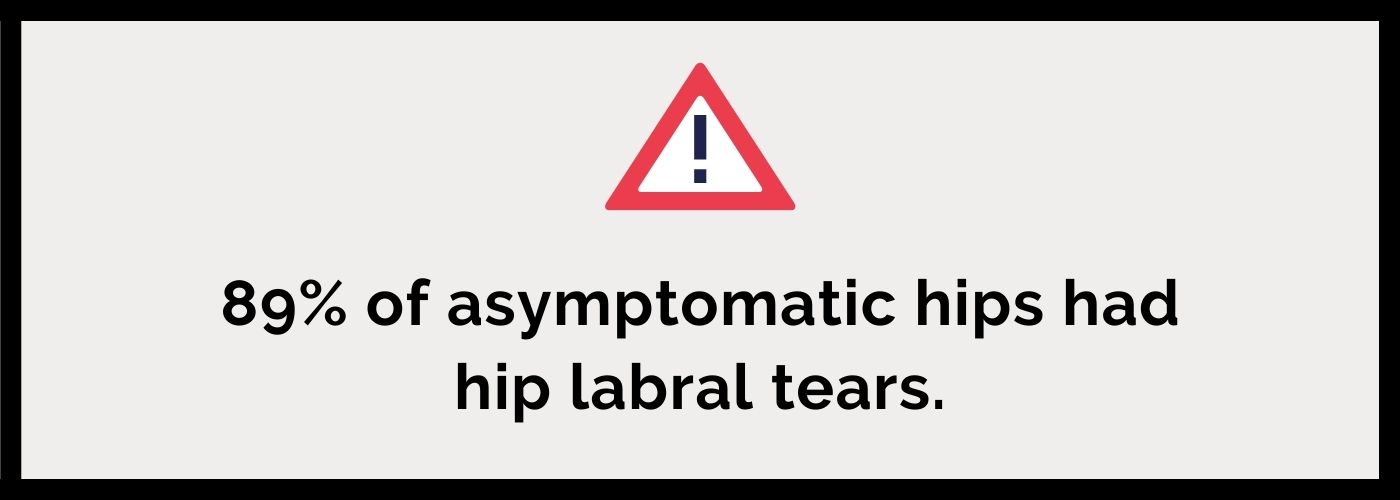
But the same rationale applies to a hip that is in pain. If there is no causation between hip pain and the hip labral tear, why would one operate on that hip? How can we be sure that the pain is coming from the hip labral tear? Especially when there is so much medical literature establishing that hip labral tears are extremely common in the general population and even more common in the athletic population?
Orthopedic surgeons MUST disclose this information to their patients. Either they don’t want to or they don’t know about this research. Either scenario is problematic and I would choose another doctor that does provide this information. I strongly believe that there are many honest doctors out there that want the best for their patients.
These are the doctors that will provide you with all the relevant information for you to make an informed decision. This is the type of doctor you want to work with. You don’t want to work with a doctor that just sees your hip as another paycheck in his wallet justified by an MRI.
And these issues with MRIs are not limited to hips. We see the same thing with other joints in the body. Scary-sounding diagnoses like shoulder labral tears, disc herniations, osteoarthritis and many others are common in the general asymptomatic population. Take a look at some of these studies:
- 72% of adults (from 45-60 years old) with no history of shoulder pain had shoulder labral tears. [Link to study].
- 57% of asymptomatic volunteers showed evidence of spinal disc pathology. [Link to study].
- Up to 43% of asymptomatic knees over 40 years old had knee osteoarthritis. [Link to Study].
In many instances, it is more common for a joint to have some type of “pathology” than not. Your hip hurt so you got an MRI on your hip which showed a labral tear. But if you got an MRI scan on your shoulder, you might find out you have a labral tear there too. But it won’t matter because your shoulder does not hurt.
Maybe labral and cartilage damage is just a completely normal and healthy progression of aging? And if we didn’t have access to million dollar MRI machines, we would just label our hip pain as…well, hip pain. And maybe the root cause of the pain has nothing to do with the labral tear at all.
Why Pain Relief from Local Injections is irrelevant to a Hip Labral Tear Diagnosis
Many orthopedic surgeons will also inject a numbing medicine into the hip along with an MRI scan. The purpose of this injection is to help with the diagnosis of a hip labral tear. If the injection alleviates the hip pain then this theoretically means that the pain is coming from the labrum. See NYU's explanation.
When I received this diagnostic injection years ago, I remember being so confused. The doctor explained that they were going to inject something into my hip and that I should pay attention to whether the pain went away.
But like many people, my pain was not constant. Everyday was different and it really depended on my activity levels. After getting the injection, I remember I couldn’t give the doctor a straight answer. I may have said something like “it helped a little bit.” That was probably enough for her to recommend surgery since the MRI also showed a labral tear.
This diagnostic tool didn’t make sense to me then and it makes even less sense to me now. Although the injection is made directly into the “hip joint,” how do we know the effect is only on the labrum?
When we go to the dentist and get a shot of novocaine, it isn’t just the tooth in question that goes numb. Our whole jaw goes numb! Couldn’t the same thing happen here? The injection numbs not just the labrum but also the surrounding area?

And finally, there is the very real risk of placebo. If a doctor tells you that you have a hip labral tear and that an injection in the hip joint will provide pain relief, then your brain and nervous system might react accordingly. The mind and nervous system are intimately connected with chronic pain patterns. So there is no question that this type of scenario can elicit a placebo response.FADIR and FABER are ineffective Tests for Hip Labral Tears
The final testing method for hip labral tears is to evaluate the range-of-motion in the hip through physical examination. There are two popular tests that are used: FADIR and FABER. FADIR stands for flexion, aDduction and internal rotation. FABER stands for flexion, aBduction and external rotation.
In both tests, the patient lays on their backs. For FADIR, the patient brings their knee up to 90 degrees, and then internally rotates the hip. “A positive test is indicated by the production of pain in the groin, the reproduction of the patient’s symptoms with or without a click, or apprehension.” See explanation from Physio-pedia.
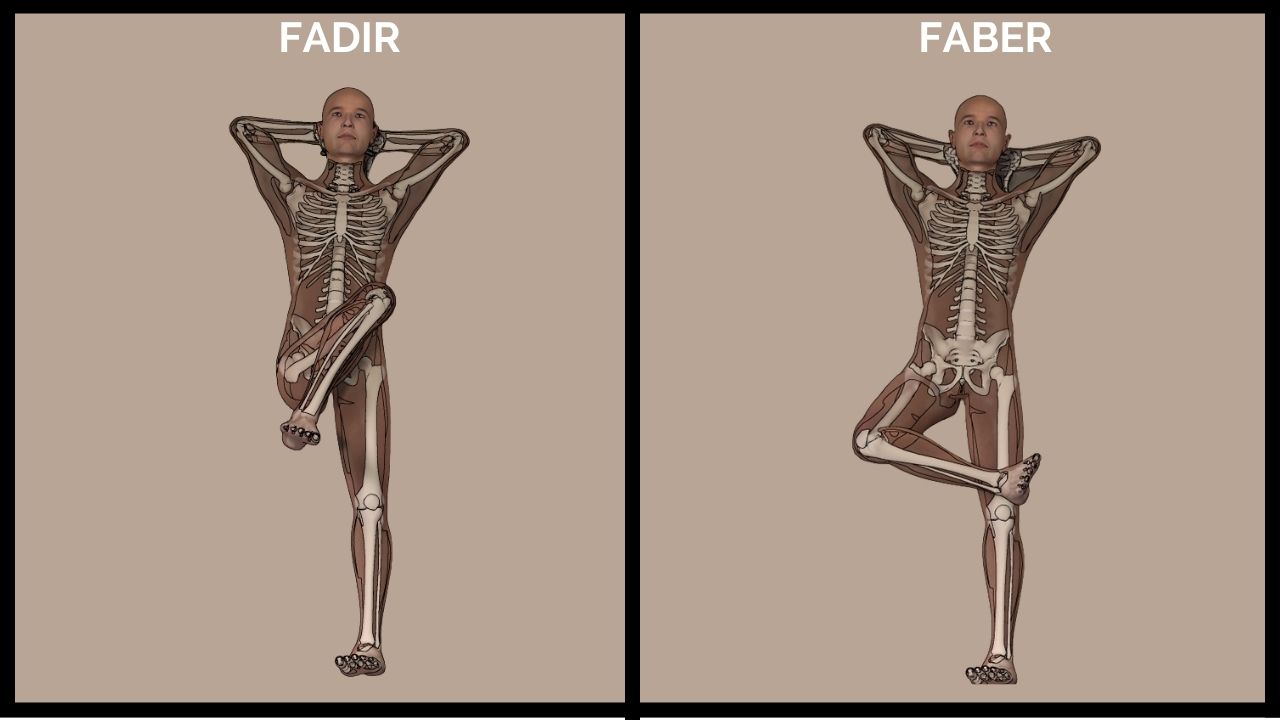
In the FABR test, aka the Patrick’s Test, the patient brings their hip into flexion and external rotation. “A positive test is one that reproduces the patient's pain or limits their range of movement.” See explanation from Physio-pedia.
Many modern humans that work behind a desk for multiple hours a day will not perform these tests well. These are difficult positions for anyone to perform, let alone someone with chronic hip pain. If I tried these tests 10 years ago when my hip pain was at its worst, I’d probably shed some tears!
However, after years of working on my hip function and strength, these positions are much more comfortable. I don’t do them with absolute perfection yet but they are MUCH better than they once were. I see the same thing with the people I work with. These positions can improve after months of rebuilding hip function.
And this is very important to understand. If you can make these movements less painful and more functional through exercise, then the poor range of motion is not due to some permanent pathology in the hip joint. And instead, the reason for testing poorly on these tests is because the muscles around the hip lack strength and flexibility in these ranges of motion.
Don’t just take my word for it. Studies examining the accuracy of these tests have confirmed their unreliability:
- FADIR test found inadequate in youth ice hockey players because of the large number of false positive test outcomes. [Link to Study].
- The FABER test has a very high risk of false positives and accuracy rates can be as low as 25%. [Link to Study].
- When combining both tests, you increase the false positive rate to 100%. [Upright Health's analysis of above study].
There is no clear path to test for hip labral tears. Each test is riddled with major issues. This is not true for other medical conditions, like gout. When I had a few flare ups in that problem joint, a doctor recommended I get my uric acid levels tested in my blood. If you have high uric acid (anything higher than 6 mg) then you are diagnosed with gout.
The path to diagnose gout is quite simple and straightforward. If you have acute bouts of an extremely painful, red, swollen big toe AND you have uric acid higher than 6 mg in your blood, you have gout. No questionable MRIs, subjective feelings of discomfort after an injection or difficult positions such as the FADIR or FABER test.We’ve now learned that many people with hip labral tears have no hip pain. We also learned that symptoms and pain patterns vary widely for the same diagnosis. And now we see that there are no reliable ways to test for hip labral tears.
The foundation for this diagnosis is starting to tumble. This level of nuance probably does not get triggered for your average person. But I’m an obsessive person and I never wanted to get an unnecessary surgery. So lucky for you, I dove head first into all of this nuance. And guess what? Things remain murky as we start examining the treatment methods for hip labral tears.
Why Conventional Treatment for Hip Labral Tears Rarely Work
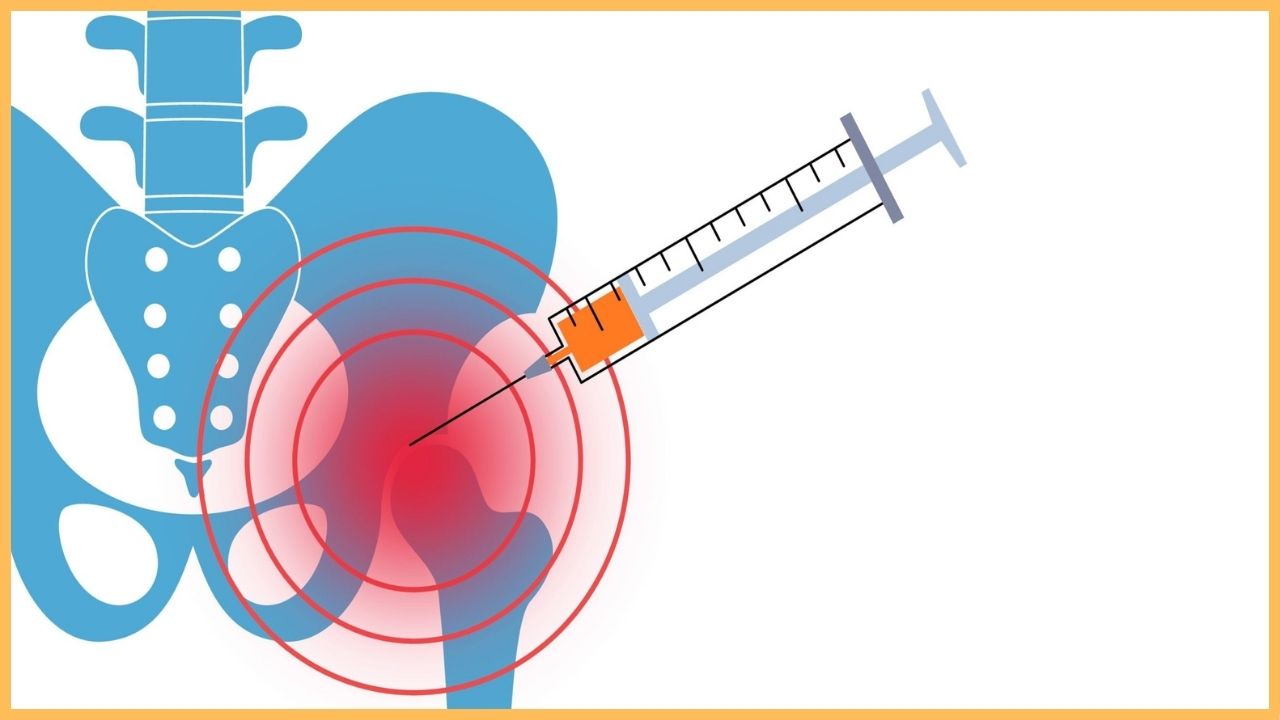
The first thing my doctor recommended after seeing my MRI with a hip labral tear was to try conservative treatment. This included steroid injections and physical therapy.
Why Steroid Injections Don’t Cure Hip Labral Tears
When you take an Advil for a toothache, it’s clear you are not getting rid of the root cause of the toothache. Advil is a pain-reliever that reduces symptoms temporarily. If you have a cavity or infection, you need a dental professional to address whatever is causing the pain.
Steroid injections act much the same. Although they provide longer-lasting relief, this type of medicine is a numbing agent. But in the world of orthopedics, local cortisone injections are treated as a mode of treatment. The first line of defense for many types of musculoskeletal pain.
I remember when I got my cortisone injection. The day of the injection I was pumped! I thought I'd get the shot and then get on the basketball court the next day. To my disappointment, the pain was still there a day after I got the injection. And the same thing happens to many clients I work with.
Medicine can be life-changing when it is the appropriate treatment for the condition. For example, the gold standard treatment for gout is a medication called allopurinol. Taking this medication daily reduces the uric acid in your blood, which is the root cause of the problem. Less uric acid = less gout attacks. The medicine is the antidote and the correct treatment.
The same cannot be said about cortisone injections for hip labral tears. At best, it numbs the area temporarily and provides short-term relief. At worst, it does nothing and a rare side effect develops. Even if there is some pain relief after an injection, think about how the nervous system will react to this.
Although we don’t like to be in pain, it is an important message we receive from our brains. It’s a sign that something is off. In the toothache example, if we keep taking pain-relievers every time the pain shows up but don’t address the root cause - the infection or cavity - the problem is only going to get worse and spread.

The same thing can occur when a cortisone injection numbs sensations of chronic hip pain. Instead of focusing on the root cause of the problem - poor movement function - we simply numb the pain sensation. We keep moving the way we always did and the structural issues in our hip continue getting worse. No bueno.
Why Physical Therapy Usually Fails for Hip Labral Tears
“Ok Maks, you said poor movement function is behind my chronic hip pain, so physical therapy must help right!?” Physical therapy seems like it would be the logical choice in treating poor movement function associated with hip labral tears. Unfortunately, this is not the case.
This is not to say there are no individual physical therapists out there that can help. Many PTs understand how poor movement function contributes to chronic hip pain and can be a valuable resource. But these PTs usually depart from the traditional PT model of care.
Traditional physical therapy helps individuals rehab certain injuries like broken bones or treat certain diseases like osteoporosis. The PT profession has been helping people improve these conditions for decades and have well established treatment protocols tested by clinical research.
But the same cannot be said about chronic and complex musculoskeletal pain. PT does not work for hip labral tears because the pain is not due to the hip labral tear. If you’ve been to a PT clinic for your hip pain, you’ll understand exactly what I’m talking about. They don’t know what to do with you.
I’ll never forget when I went to my third PT office back in 2013 and one of the clinicians said “Oh, you got FAI and a hip labral tear. Only way to get rid of that is surgery.” And this casual statement by a young PT perfectly summarizes why PT is inappropriate for treating hip labral tears and chronic hip pain.
PT operates under the surgical model. It is treated as a stop-gap before doing the thing that everyone believes actually helps - surgery. There are no assessments of how your hips move. There is no analysis of how your body functions. They just throw you on a leg press machine and have you do a few reps before surgery.
Think twice before Hip Labral Tear Surgery
The last option in conventional treatment for hip labral tears is arthroscopic hip surgery. There are a few objectives with this type of surgery. The first is to reattach the torn labrum to the socket if possible. The second is to trim or smoothen the area of the labrum that is frayed. [Link to Source].
And the third objective is to “fix” the bony abnormalities that theoretically caused the labrum to tear. These bony abnormalities are the basis of FAI (aka femoroacetabular impingement) which is usually a diagnosis that accompanies a hip labral tear. This is accomplished by shaving down the bony rim of the acetabulum and/or the bump on the femoral head. [Link to Source].
As we’ve seen, many people who have hip labral tears don’t have hip pain. The same is true for FAI. Many people have bony abnormalities constituting FAI but don’t have hip pain. Here are some studies to drive this home:
- 25% of 244 men with no history of hip pain had FAI.
- Meta-review analyzing 2,114 asymptomatic hips found FAI in 67% of hips.
- 57% of asymptomatic Korean men had FAI.
- 72% of 110 asymptomatic hips had signs of FAI.
FAI is diagnosed when there is not a “perfect” fit between the femur and the acetabulum. But what makes us think that this fit should be perfect? FAI only started getting diagnosed in the 1990s. Do we think the femur perfectly fit into each person’s acetabulum before the orthopedic field invented the FAI diagnosis?
The basis for hip labral tear surgery is to create this perfect fit between the femur and acetabulum. This will allegedly heal the labrum and prevent future damage to the labrum. If this is true, then we would expect high labral tear surgery success rates. Unfortunately, the research does not demonstrate this:
- Expectations for pain relief were not met for half of study participants getting surgery for FAI. [Link to Study].
- Over one-third of patients were unsatisfied with surgical outcomes for FAI. [Link to Study]. [Link to Upright Health's review of this study].
There are not many good studies analyzing success rates for these types of surgeries. As Matt Hsu from Upright Health explains, the way the studies are set up makes it easy to skew the results in a way that favors surgical intervention.
For example, in the second study above, 64% of study participants reported satisfaction with their surgical outcome. But this was only based on a minor improvement in a questionnaire that was provided before and after the surgery. A slight global improvement in a questionnaire does not mean most of the individuals getting surgery were no longer in hip pain.
By itself, the research on labral tear surgery success rates is inconclusive. Maybe some people get positive results while others get poor results. But I think it’s important to look at the whole picture. There is grayness in each aspect of the hip labral tear diagnosis.
The symptoms, the testing and the treatment for hip labral tears are all suspect. There is no cohesive path from diagnosis to treatment. Why do some people with hip labral tears have pain while others don’t? Why do some people get pain-relief from steroid injections while others need surgery? The answer you usually get from doctors is that they don’t know.
This speculation taken as a whole should make you seriously question this diagnosis. And the next section will provide an alternative and rational way to start troubleshooting your chronic hip pain.
What a Healthy and Functional Hip Labral Tear Recovery Looks Like
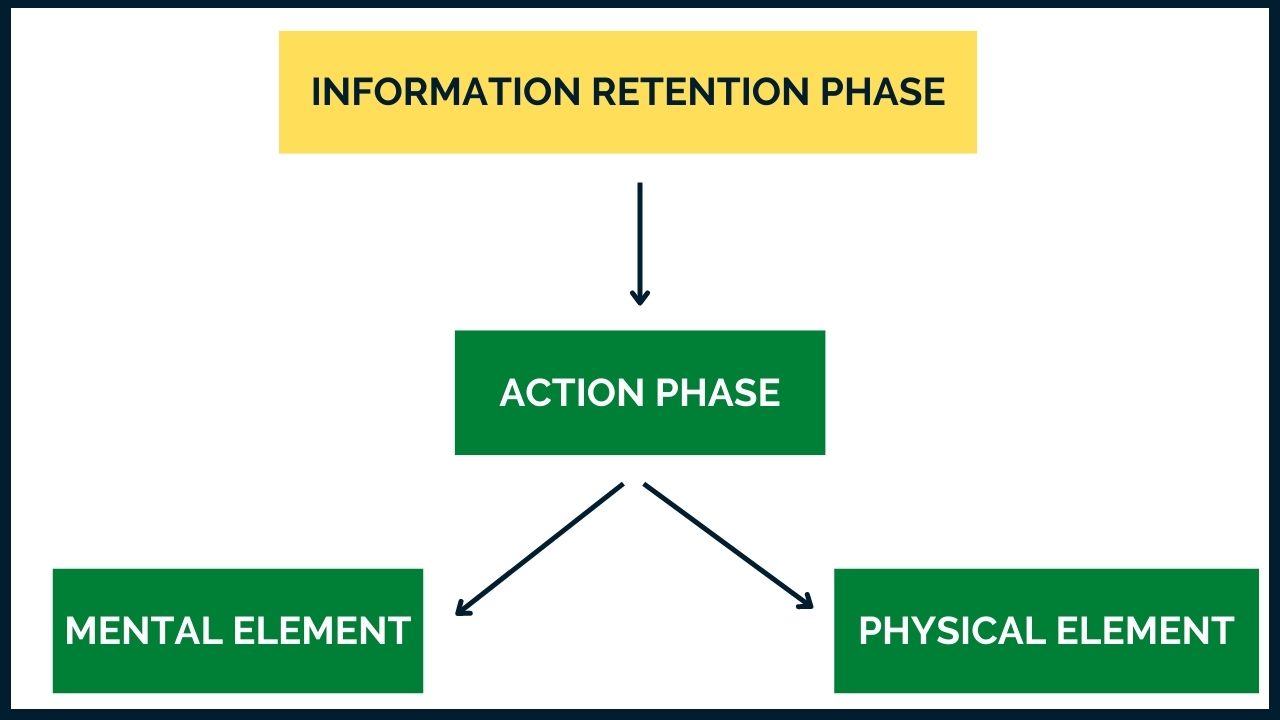
If you are reading this article, you are probably still in the information retention phase. This is where you are researching and learning everything you possibly can about hip labral tears. This is an important step. But eventually, you want to move into the action phase.
When going into the action phase, it is so critical to not dive too deep, too soon. I see so many people get so excited about solving their hip issues through exercise that they set unrealistic expectations for themselves. They think they can get rid of their chronic hip pain in weeks or even a few months.
One of my mentors says: “the way you’re feeling is a reaction to how you’re loading.” Hip pain is a result of how your entire musculoskeletal system holds itself up and fights gravity. These are movement habits that you’ve used for years. When you enter the world of movement training, you are not just getting rid of hip pain. But instead, improving how your entire body functions and moves.
So it takes time. But not just a certain amount of days, weeks or months. But time to build body awareness. To understand why your body feels the way it does. Hip pain can be the result of how your opposite hip functions, how your shoulders function or how your ankles and feet function.
But everyone needs a place to start. And I think there are two critical elements when you are shifting into the action phase.
The Mental Element of Hip Labral Tear Recovery
Most people searching for hip labral tear relief are very much still in the medical mindset of physical healing. In other words, the hip pain is because of a hip labral tear. And because this is a medical condition, you need some type of ‘fix”, or antidote. In medicine, it is injections and surgery but it can also manifest itself in corrective exercise.
For example, one may believe that a certain muscle is to blame for the hip pain and that by releasing or strengthening it, the pain will go away. Or that there is a certain set of exercises that if done in perfect sequence, will heal the pain for good.
This was how I approached my movement practice for a long time. But I eventually realized that the same desperate energy I had seeking answers in the medical world, I brought into the movement world. I wanted to know what that one thing was that was causing my pain. The one thing I can fix.
I finally realized that my hip pain was a culmination of many things. How I sit, how I walk, how I hold myself up and how I respond to pain signals. There was no “one thing” because it was “everything.” It wasn’t the hip labral tear that was causing me pain but how I interacted with my environment every single minute of every single day.
It is difficult to pull away from the belief that your hip pain is due to your hip labral tear. Or from the way your bones are shaped. But if the mind is stuck on the false belief that the hip can only be fixed through surgery then this will dictate your experience. There needs to be a letting go of this false storyline. Otherwise, any time anything is felt in the hip, the mind will go directly back to this false narrative.
This point is at the heart of this article. The fear of the hip labral tear diagnosis is worse than the diagnosis itself. A torn labrum sounds like some scary and horrible thing but it’s really not. We don’t need to fix a hip labral tear in order to be out of chronic hip pain. This is the crucial mindset shift that needs to happen before diving into a comprehensive movement practice.
That is why I focus on the psychological element with each person I work with. It is not if the mind is involved in your pain pattern, but how. Diving into a movement practice without this recognition is a recipe for disaster.
The hip labral is there. And it might always be there. But that does not mean it is why you are in pain. Or that you need surgery. If we develop a healthier relationship to pain, we understand it is not some boogie man that is trying to take over our life. Instead, it is just a messenger telling us we need to integrate some better balance in our bodies and movement.
The Physical Element of Hip Labral Tear Recovery
As important as the psychological element is, you cannot think your way out of chronic hip pain. The brain is letting you know that there is something about the way your body moves and functions that is making your hip hurt. But the only way to understand what is causing this pain signal is to become more educated on how your body is supposed to move.
Movement education is critical. We need to learn how hips are supposed to function and in what ways our hips cannot. We also need to examine what the ankles, knees and shoulders are doing. This is because human movement is done through multi-joint function and not just in the joints that hurt.
But what type of movement practice do you need? How do you get started? The answer is somewhere. Find coaches and resources that you trust and try things out. Every training experience is an opportunity to learn more about your body. To bring back function into your hips.
I’ve tried so many different modalities through the years and definitely have found things that work for me. But sometimes I don’t know how much one thing helped more than another. I’ve been training my hips for a decade. When I find some great new training program, is it the new program that helped or is it everything that got me to that point?
Good enough is better than perfect. And although the best type of training might be 1-on-1 in person with a great coach, you can get a lot done at home following along with an online program. What you’re looking for is more aha moments. Where you notice enough of a difference in your hips that you start seeing the light. Your pain might not be gone but you know something has changed in your movement and body. You see the light even though it's still very distant. This is what propelled me years ago.
Closing Thoughts
My hip pain was once terrible. I couldn’t play sports. I couldn’t hike. I couldn’t even sit on a couch and watch TV. But then I mentally and physically committed to using movement to work my way out of hip pain. And after a few months, I noticed changes. A few years, even more changes.
10 years later, I am not in this type of pain anymore. I am active. I play sports. I hike and I do whatever physical activity I want. But the movement practice continues. I still notice stiffness. I notice tightness. I get pain in other areas sometimes.
That’s because I’m a human living in the 21st century. Where for the first time in mankind, we need to deliberately make time to create movement in our lives. Charles Darwin says “It is not the strongest of the species that survives, nor the most intelligent. It is the one most adaptable to change.”
Modern day humans need to adapt to the non-existent stimuli for movement. If we live our lives without intentionally making time to create that stimuli, pain, stiffness and joint degeneration is inevitable.

